These states have the highest-quality home health agencies, according to patients
Published 2:30 pm Wednesday, April 24, 2024
These states have the highest-quality home health agencies, according to patients
In an ideal world, at-home health care services would be equal no matter where a patient lives—after all, these services transfer care into the comfort of one’s own home. But the reality is far from balanced.
The need for home health aides is expected to balloon over the next several years. This increased demand is in part because populations in many areas are aging. In New York, for instance, the number of home aides who provide at-home health services has more than doubled over the past 10 years, totaling over 500,000. Over the coming decade, it is expected that more new jobs will open in the home care occupation than in any other industry.
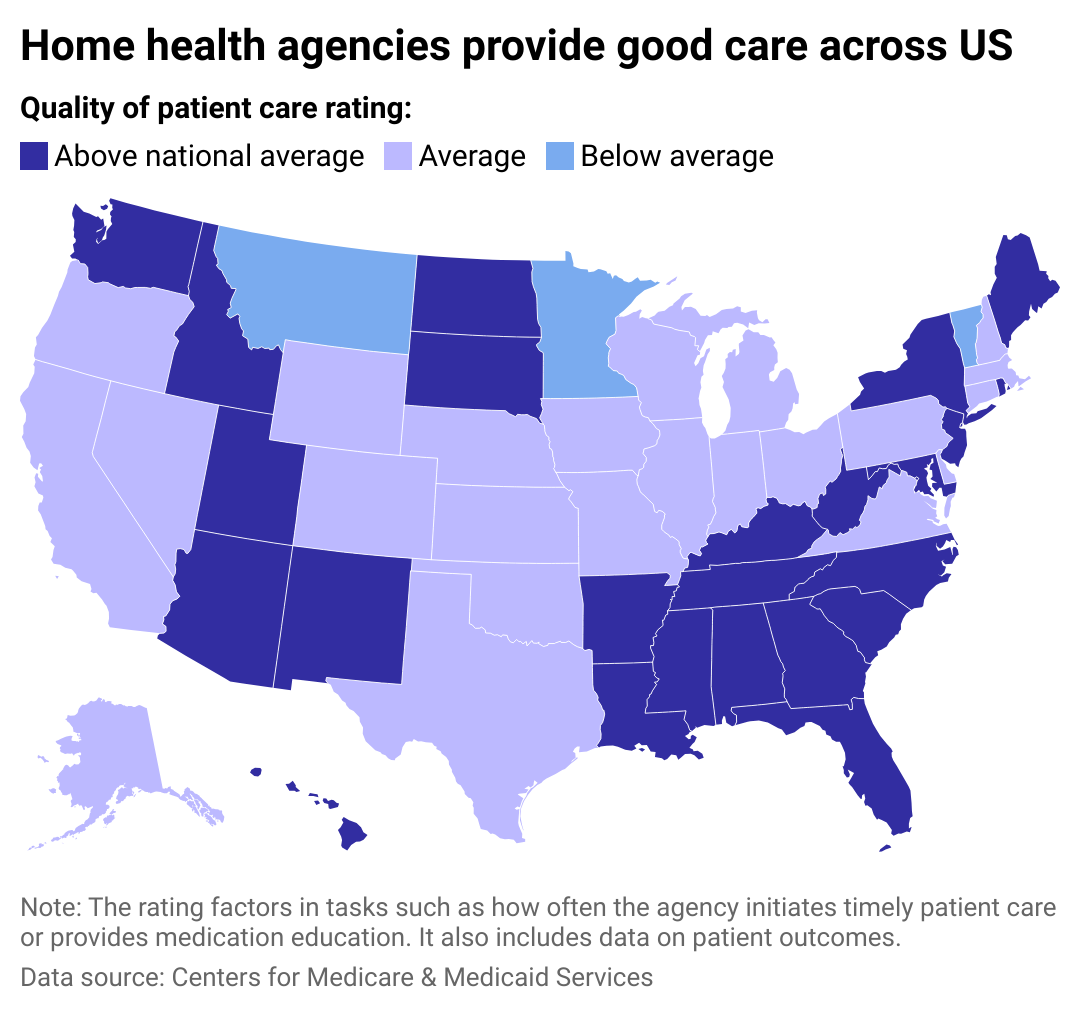
Vivian Health visualized data from the Centers for Medicare & Medicaid Services to identify states with the highest- and lowest-rated home health agencies. The ratings address the quality of patient care, ranging from 1-5.
![]()
Vivian Health
Only 3 states rated below average for patient care
The location where someone lives can play a big role in both the care patients have access to and the resources that home health aides receive. Southern and Southeastern states make up the majority of the states with the highest home health care ratings: Mississippi, West Virginia, Tennessee, South Carolina, Louisiana, Kentucky, and Alabama. Costs can range dramatically from state to state—for instance, Mississippi’s monthly average for in-home health services is $3,800, while Massachusetts is around $6,000. Montana, Minnesota, and Vermont rated below average for quality of home health patient care.
For those in rural areas, care providers might have to travel further to reach patients, and there may not be as many medical resources available, resulting in a lower quality of care when compared to urban areas.
The inequities in at-home services also mirror the disparities present in the health care system at large: Black and Hispanic patients, as well as patients from low-income or marginalized neighborhoods, are less likely to receive high-quality at-home health care than white and/or higher-income patients.
The agency facilitating services can also play a pivotal role in determining how successful at-home health care may be for a patient. Their task begins with pairing patients with their in-home aide, determining the schedule and frequency of care, and arranging appropriate services. Crucially, agencies can act as an intermediary between a patient and their primary physician, who is now seeing the patient far less than if they were in a facility.
While the home health care industry still remains largely unregulated, that isn’t expected to last for long. Private equity firms are rushing to claim their stake in what promises to be a lucrative market. States are increasingly recognizing that the hours at-home aides work—and the minimum wage they earn—need to be reevaluated. In just a few years, access to and funding for home health care may be completely transformed—hopefully, in a direction that balances the scales for consumers.
Home health care coverage
Just what “home health care” is can encompass a wide range of services and can often be confused with “home care.” While the latter helps ill and/or disabled individuals live more comfortably and safely day to day, home health care uses clinical methods to directly treat injuries and illnesses. Care can range from injections to occupational therapy to wound care and is often authorized for a set term following a patient’s medical procedure or for seniors with chronic conditions and those who want to age in place.
Reflecting these complexities, Medicare only covers home health care, and only within certain parameters. As of March 2024, New York lawmakers are battling over a proposal that would consolidate—and ostensibly limit the scope—of Medicaid’s consumer-directed personal assistance program, or CDPAP, which supports individuals opting for home care.
Figuring out who funds home health care, and to what extent, is a time-pressed task. Particularly following the havoc COVID-19 wreaked in nursing homes, many older Americans are opting to live at home, rather than in assisted living facilities. This desire goes for those with disabilities or chronic illnesses, as well as those undergoing end-of-life care. Besides a higher sense of safety for many, at-home health care is also attractive for providing a stronger sense of independence and decreasing experiences of loneliness.
Story editing by Shannon Luders-Manuel. Copy editing by Tim Bruns.
This story originally appeared on Vivian Health and was produced and
distributed in partnership with Stacker Studio.






